Module 2. Life-Threatening Emergencies
What is a Breathing Emergency?
A breathing emergency is any situation where a person experiences difficulty breathing or their breathing becomes severely impaired. Without quick action, this can rapidly become life-threatening.Common Causes of Breathing Emergencies
- Asthma – Inflammation and narrowing of the airways causes wheezing and shortness of breath.
- Choking – A blocked airway prevents normal breathing.
- Severe Allergic Reaction (Anaphylaxis) – Swelling of the airway can restrict or stop breathing entirely.
- Heart Attack – May cause shortness of breath due to reduced blood flow to the lungs.
- Lung Infections – Pneumonia and bronchitis can compromise breathing capacity.
- Trauma – Injury to the chest or lungs can impair breathing mechanics.
- Chronic Conditions – Long-term effects of smoking may cause COPD and other respiratory issues.
- Inhaled Toxins – Fumes, smoke, or carbon monoxide can interfere with oxygen exchange.
Recognizing Breathing Distress
Mild to Moderate Symptoms
- Shortness of breath
- Wheezing or audible whistling while breathing
- Persistent, uncontrollable coughing
Severe Symptoms (Life-Threatening)
- Very fast or very slow breathing rate
- Pale, blue, or gray skin—especially around the lips (cyanosis)
- Confusion, lightheadedness, or slurred speech
- Chest pain or pressure
- Gasping or inability to speak
Responding to a Breathing Emergency
1. Assess the Scene and the Victim
- Check for safety before approaching.
- If the person is conscious, ask about symptoms and medical history.
- If unconscious and not breathing normally, begin CPR.
2. Assist with Prescribed Medications (If Applicable)
- Asthma: Help them use a rescue inhaler.
- Allergic Reaction: Assist with an epinephrine auto-injector (EpiPen).
- Chest Pain: Offer prescribed heart medication, such as nitroglycerin, if available.
3. Call 911 If Any of the Following Apply
- Breathing doesn’t improve with medication.
- The person cannot speak or breathe normally.
- The skin turns blue, gray, or very pale.
- The person collapses or becomes unresponsive.
4. Make the Person Comfortable
- Loosen tight clothing around the chest and neck.
- Help them sit upright—this can ease breathing.
- Remain calm and reassuring to reduce anxiety.
5. Be Prepared to Start CPR
- If the person stops breathing or becomes unresponsive, begin CPR immediately and continue until help arrives.
Using an Inhaler (Asthma Attack)
- Shake the inhaler well before use.
- Remove the cap and have the person exhale completely.
- Place the mouthpiece into their mouth and create a tight seal.
- Press down on the inhaler as they inhale slowly and deeply.
- Have them hold their breath for 10 seconds, then exhale slowly.
- Repeat after 30–60 seconds, if needed.
Key Takeaways
- Breathing emergencies may result from asthma, choking, anaphylaxis, cardiac issues, or lung infections.
- Signs such as cyanosis, gasping, and confusion require immediate medical attention.
- Support the victim with their medication if available.
- Call EMS if breathing does not improve or if severe symptoms are present.
- Be prepared to initiate CPR if the victim stops breathing.
What Is Carbon Monoxide Poisoning?
Carbon monoxide (CO) poisoning occurs when a person inhales excessive CO gas, which displaces oxygen in the body and prevents normal cellular function. Because CO is odorless, colorless, and tasteless, it cannot be detected without a CO detector—making it especially dangerous. Carbon monoxide poisoning is a medical emergency. Without prompt action, it can lead to brain damage, unconsciousness, or death.Common Sources of Carbon Monoxide
- Faulty gas appliances (heaters, stoves, ovens, furnaces, water heaters, fireplaces)
- Running a car in an enclosed garage
- Blocked chimney vents or damaged exhaust systems
- Indoor use of generators or charcoal grills
- Kerosene heaters, propane stoves, or gas-powered tools operated without ventilation
Signs and Symptoms
Mild to Moderate Exposure
- Headache, dizziness, or nausea
- Shortness of breath or confusion
- Fatigue, blurred vision, or chest discomfort
- Loss of coordination or fainting
Severe Exposure
- Seizures or convulsions
- Loss of consciousness (coma)
- Blue or cherry-red skin (signs of hypoxia)
- Cardiac or respiratory arrest
What to Do in a Carbon Monoxide Emergency
Step 1: Remove the Person from Exposure
- Immediately move the individual into fresh air.
- If indoors, open windows and doors; turn off potential sources of CO (appliances, generators).
- Do not re-enter the environment until it is confirmed safe by emergency personnel.
Step 2: Call Emergency Services
- Dial 911 as soon as the person is in fresh air.
- Even if symptoms improve, medical evaluation is required.
- Advanced treatment may include 100% oxygen or hyperbaric oxygen therapy.
Step 3: Monitor and Support
- If the person is unresponsive and not breathing, begin CPR.
- If breathing is present, monitor closely and keep them calm and still.
When to Call 911
- Symptoms include dizziness, weakness, or fainting.
- Multiple individuals in the same environment report feeling ill.
- The person is unconscious or not breathing.
How to Prevent Carbon Monoxide Poisoning
- Install CO detectors near all sleeping areas and in key locations throughout the home.
- Have gas-burning appliances and fireplaces inspected annually.
- Never run a vehicle or gas-powered tool inside a garage or enclosed space.
- Avoid using grills, generators, or portable heaters indoors.
- Evacuate immediately if a CO alarm sounds, and call emergency services.
Key Takeaways
- Carbon monoxide is undetectable without a CO alarm and can be deadly.
- Move victims to fresh air and contact emergency services immediately.
- Initiate CPR if the person is unresponsive and not breathing.
- Prevention is critical: use CO detectors and ensure proper ventilation.
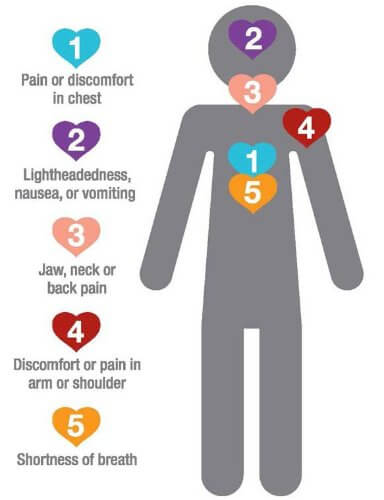
What Is a Heart Attack?
A heart attack (myocardial infarction) occurs when blood flow to part of the heart is blocked, usually by a clot or plaque. This deprives the heart muscle of oxygen, causing tissue damage. Without prompt treatment, the damage can become permanent and lead to cardiac arrest or death.
Heart attacks are medical emergencies—early recognition and intervention significantly improve outcomes.
Signs and Symptoms
×
Signs and Symptoms
 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved
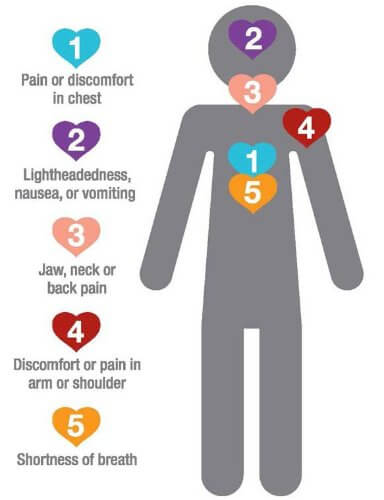
- Chest discomfort: pressure, squeezing, tightness, or pain
- Pain that radiates to the arms, jaw, back, neck, or upper stomach
- Shortness of breath (with or without chest pain)
- Nausea, vomiting, or cold sweats
- Lightheadedness, fainting, or extreme fatigue
Note: Women, older adults, and people with diabetes may experience symptoms that are less obvious, such as fatigue, back pain, or indigestion.
First Aid for a Suspected Heart Attack
Step 1: Call 911 Immediately
- Do not wait to see if symptoms improve—time is critical.
Step 2: Help the Person Rest
- Have them sit or lie in a comfortable position.
- Loosen tight clothing to ease breathing.
- Offer reassurance to keep them calm and reduce anxiety.
Step 3: Administer Aspirin (If Safe)
- If the person is not allergic and has no contraindications, offer one adult (325 mg) or two low-dose (81 mg) aspirins to chew and swallow.
- Do not give aspirin if they have been advised by a doctor to avoid it.
Step 4: Be Prepared for Cardiac Arrest
- If the person becomes unresponsive or stops breathing, begin CPR immediately.
- Start chest compressions—at least 100–120 per minute, in the center of the chest.
- If an automated external defibrillator (AED) is available, use it as directed.
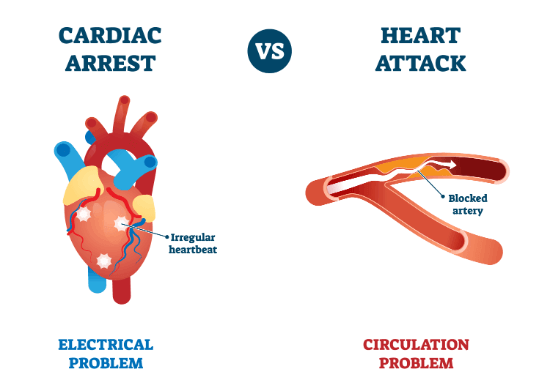
Heart Attack vs. Cardiac Arrest
×
Heart Attack vs. Cardiac Arrest
 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved
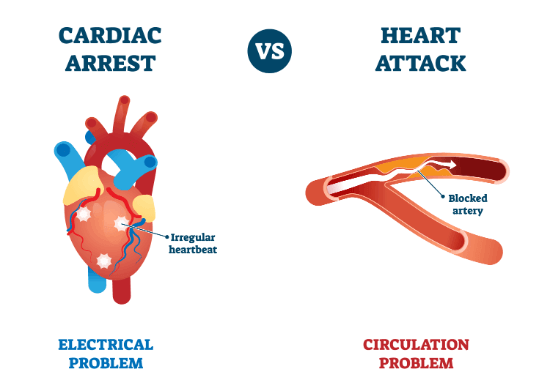
- Heart attack: Blood flow to the heart is blocked. The heart may still be beating. Treatment is urgent but may not involve CPR unless breathing stops.
- Cardiac arrest: The heart stops beating. The person is unresponsive and not breathing. Immediate CPR and defibrillation are required.
When to Call 911
- Chest pain lasts longer than five minutes or comes and goes
- Pain spreads to arms, back, jaw, or stomach
- Shortness of breath, fainting, or sudden fatigue
- Person becomes unresponsive or stops breathing
Key Takeaways
- Heart attacks are caused by blocked blood flow to the heart muscle.
- Call 911 at the first signs of a possible heart attack—do not delay.
- Assist with aspirin if appropriate, and help the person stay calm and at rest.
- If they stop breathing, begin CPR and use an AED if available.
What Is Choking?
Choking occurs when a foreign object blocks the airway, preventing normal breathing. While food is the most common cause, choking can also result from small objects, liquids, or swelling due to allergic reactions. Prompt recognition and intervention are essential.
How to Recognize Choking
If the Person Can Cough or Speak
- The airway is partially blocked.
- Encourage continued forceful coughing to expel the object.
- Do not intervene with abdominal thrusts unless the person can no longer breathe.
If the Person Cannot Cough, Speak, or Breathe
- This is a complete airway obstruction and a medical emergency.
- Look for the
universal choking sign
—hands clutching the throat.×universal choking sign
 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved - The person may appear panicked, turn blue (cyanosis), or lose consciousness.
First Aid for Adults & Children (Over Age 1)
Heimlich Maneuver (Abdominal Thrusts)
- Confirm they are choking and unable to speak or breathe.
- Stand behind the person and place one foot between theirs for balance.
- Wrap your arms around their waist and make a fist just above the navel.
-
Grasp your fist with your other hand
×Grasp your fist with your other hand
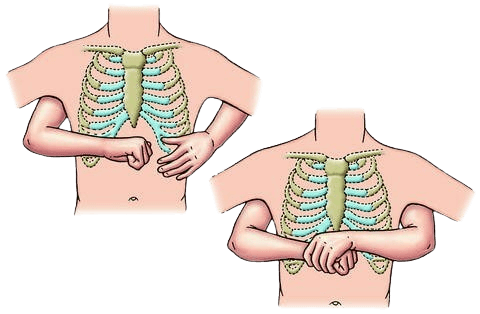 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved
and deliver quick, upward thrusts. - Repeat until the object is expelled or the person becomes unresponsive.
If the Person Becomes Unresponsive
- Lower them to the ground.
- Call 911 and begin CPR if they are not breathing.
First Aid for Infants (Under Age 1)
Do Not Perform the Heimlich Maneuver on Infants.
Use alternating back blows and chest thrusts instead:
- Position the infant face down on your forearm, supporting the head and neck. Keep the head lower than the chest.
-
Deliver 5 firm back blows
×Deliver 5 firm back blows
 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved
between the shoulder blades using the heel of your hand. - Turn the infant face up while maintaining head support.
-
Give 5 chest thrusts
using two fingers placed just below the nipple line, pressing down approximately 1.5 inches.×Give 5 chest thrusts
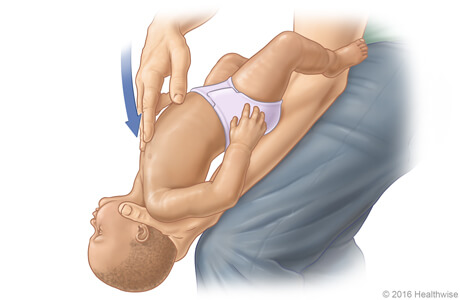 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved - Repeat cycles of 5 back blows and 5 chest thrusts until the object is expelled or the infant becomes unresponsive.
If the Infant Becomes Unresponsive
- Call 911 and begin infant CPR immediately.
When to Call 911
- The person cannot breathe, cough, or speak.
- The person becomes unconscious.
- The object remains lodged after multiple attempts.
- The infant is unresponsive or lethargic, even if the object is dislodged.
After choking, monitor for difficulty breathing or swallowing. Seek medical evaluation even if the person recovers fully.
Key Takeaways
- If the person can breathe or speak, encourage coughing—do not intervene prematurely.
- If they cannot breathe, cough, or speak, perform the Heimlich Maneuver immediately.
- Infants require back blows and chest thrusts, not abdominal thrusts.
- Call 911 if the airway remains blocked or the person becomes unresponsive.
Understanding Drowning
Drowning occurs when water prevents the lungs from getting oxygen, leading to suffocation. Even if a drowning victim is revived, they may suffer brain damage or death from prolonged oxygen deprivation.
Drowning is often silent. Victims may not splash or yell—they frequently slip beneath the surface quietly.
Common Drowning Locations
- Pools, lakes, oceans, or rivers
- Bathtubs (especially for children)
- Buckets or toilets (in small children)
Recognizing Drowning
- Head tilted back with mouth open
- Weak arm movement or flailing
- Glassy, panicked, or closed eyes
- Struggling to stay afloat without progress
- Quiet or unable to call for help
If a person disappears underwater, respond immediately.
First Aid for Drowning
Step 1: Remove the Person from the Water Safely
- Do not put yourself in danger.
- Use a reaching tool (rope, flotation device, stick) if available.
- If entering the water, approach from behind to avoid being grabbed.
Step 2: Check for Breathing and Pulse
- If the person is not breathing, begin CPR immediately.
- If breathing, place them on their side (recovery position).
- All drowning victims should be evaluated by a medical professional—even if they regain consciousness.
Step 3: Perform CPR if Necessary
- Begin with 2 rescue breaths (since oxygen loss is the primary issue).
- Follow with 30 chest compressions, then 2 breaths—continue until help arrives or the person recovers.
Delayed Complications: Dry and Secondary Drowning
- Symptoms may develop hours after the incident.
- Watch for coughing, difficulty breathing, or extreme fatigue.
- Seek emergency care even if the person appears fine initially.
When to Call 911
- The person was submerged or unresponsive.
- They are not breathing or need CPR.
- They regain consciousness but show difficulty breathing or other symptoms.
Prevention Tips
- Never leave children unattended near water.
- Learn CPR and keep your skills current.
- Always wear life jackets in natural bodies of water.
- Never swim alone.
- Avoid alcohol or drugs while swimming or boating.
- If someone is in trouble, throw them a flotation device instead of jumping in.
Key Takeaways
- Drowning is often silent—know the signs and stay alert.
- Remove the person from water safely and begin CPR if needed.
- All victims should receive medical attention to rule out secondary complications.
- Prevention through supervision and safety measures is essential.
What Is a Seizure?
A seizure is a sudden, uncontrolled electrical disturbance in the brain. It may cause convulsions, loss of consciousness, confusion, or unusual behavior. Seizures can last seconds to several minutes and may be triggered by:- Epilepsy (chronic seizure disorder)
- Head trauma or brain injury
- High fever (febrile seizures in children)
- Stroke or low oxygen levels
- Low blood sugar (hypoglycemia in diabetics)
- Drug or alcohol withdrawal
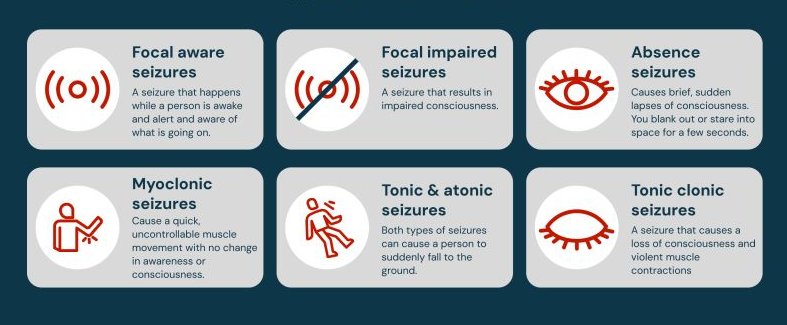
Types of Seizures
×
Types of Seizures
 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved
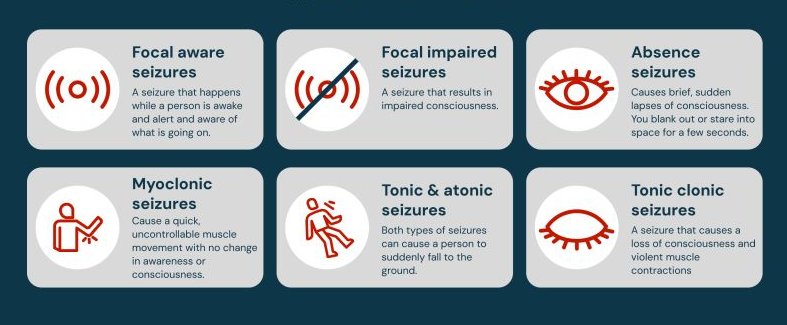
- Generalized Seizures (Tonic-Clonic / Grand Mal)
- Full-body convulsions, loss of consciousness
- May last 30 seconds to 2 minutes
- Absence Seizures (Petit Mal)
- Brief episodes of staring or unresponsiveness
- No convulsions—often mistaken for daydreaming
- Focal Seizures (Partial Seizures)
- Jerking, confusion, or unusual sensations
- Person may remain conscious but unable to respond
First Aid for Seizures
What to Do
- Stay calm and protect the person from injury
- Guide them gently to the ground, if needed
- Clear the area of sharp or dangerous objects
- Loosen clothing around the neck
- Place something soft under their head
- After the seizure, roll them onto their side to prevent choking
- Stay with them until they are fully alert
What NOT to Do
- Do NOT hold the person down
- Do NOT put anything in their mouth
- Do NOT offer food, drink, or medicine immediately after the seizure
- Do NOT perform CPR unless they stop breathing after the seizure ends
When to Call 911
- The seizure lasts longer than 5 minutes
- The person has repeated seizures without regaining consciousness
- They are injured during the seizure
- This is their first known seizure
- The person does not regain consciousness after the seizure ends
First Aid for Febrile Seizures (Children)
Febrile seizures are triggered by high fever in children under age 5. Most last under 5 minutes and resolve on their own.- Gently lay the child on their side in a safe space
- Do not put anything in their mouth or attempt to stop movement
- Remove excess clothing to cool them down
- Monitor breathing and contact a doctor after the seizure
Key Takeaways
- Seizures range from staring spells to full convulsions
- Most seizures stop within minutes and don’t require emergency care
- Protect the person, stay calm, and never put anything in their mouth
- Call 911 if the seizure is prolonged, repeated, or causes injury
What Is Shock?
Shock is a life-threatening condition where blood circulation fails to deliver adequate oxygen to vital organs. Without prompt treatment, it can result in organ failure or death.
All forms of shock are considered medical emergencies.
Primary Causes of Shock
- Severe blood loss – from trauma or internal bleeding
- Excessive dilation of blood vessels – as seen in severe allergic reactions (anaphylaxis)
- Heart failure – when the heart cannot effectively pump blood
Types of Shock
×
Types of Shock
 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved

- Hypovolemic Shock – due to severe bleeding, burns, or dehydration
- Cardiogenic Shock – caused by heart attacks or heart disease
- Neurogenic Shock – resulting from spinal cord injuries
- Septic Shock – triggered by serious bloodstream infections
- Anaphylactic Shock – a severe allergic reaction that causes airway constriction and circulatory collapse
Signs & Symptoms
- Dazed or confused appearance
- Pale, cold, or clammy skin
- Weak, rapid pulse
- Shallow or irregular breathing
- Nausea or vomiting
- Thirst, dizziness, or dilated pupils
- Loss of consciousness (in advanced cases)
First Aid for Shock
Step 1: Positioning
- Lay the person flat on their back.
- Elevate legs about 12 inches unless injury prevents it.
Step 2: Ease Breathing
- Loosen tight clothing.
- Do not move the person unnecessarily.
Step 3: Maintain Body Temperature
- Cover with a blanket or jacket to prevent heat loss.
- Keep them calm to reduce stress.
Step 4: Monitor & Respond
- Watch for changes in breathing or pulse.
- Turn on side if vomiting or unresponsive.
- Begin CPR if breathing stops.
Step 5: Call 911
- Shock always requires emergency medical attention.
- Do not give food, drink, or medication.
Anaphylactic Shock
×
Anaphylactic Shock
 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved

Anaphylaxis is a severe allergic reaction that can block airways and lower blood pressure rapidly.
Key Signs
- Skin rash or hives
- Facial or throat swelling
- Shortness of breath or wheezing
- Chest tightness
- Weak pulse or confusion
Immediate Actions
- Use an
EpiPen
(if available) immediately.×EpiPen
 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved - Call 911 regardless of symptom improvement.
- Help the person sit upright to aid breathing.
- Monitor for CPR needs if condition worsens.
Fainting vs. Shock
Fainting is a short-term loss of consciousness due to a drop in blood flow to the brain and may signal early shock.
- Help the person sit or lie down with legs elevated.
- If unconscious for more than one minute, call 911.
When to Call 911
- The person shows signs of shock (pale, rapid pulse, altered consciousness).
- They lose consciousness and do not wake quickly.
- They experience symptoms of a severe allergic reaction.
- They stop breathing—start CPR if necessary.
Key Takeaways
- Shock is a critical failure of circulation that can become fatal quickly.
- Causes include trauma, illness, allergic reactions, and dehydration.
- Keep the person warm, calm, and lying down. Do not give food or drink.
- Call 911 for all cases of shock.
- Use an EpiPen immediately for anaphylaxis and be ready to give CPR.
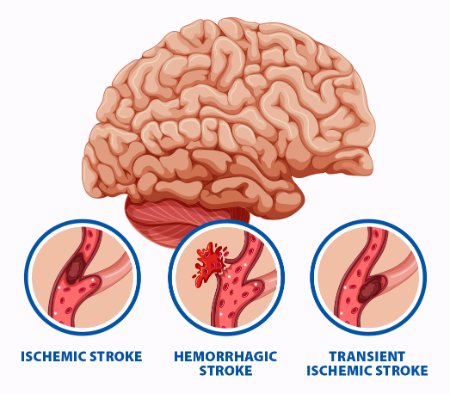
What Is a Stroke?
A stroke occurs when blood flow to the brain is interrupted—either by a blocked artery (ischemic stroke) or a ruptured blood vessel (hemorrhagic stroke). Without oxygen, brain cells begin to die within minutes.
All strokes are medical emergencies. Immediate action is critical to reduce brain damage and improve recovery.
Types Of Stroke
×
Types Of Stroke
 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved
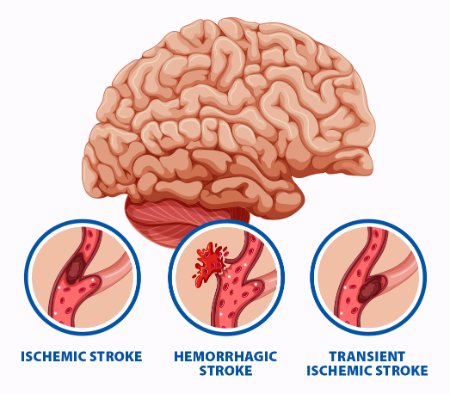
- Ischemic Stroke – Caused by a blood clot blocking an artery in the brain (most common).
- Hemorrhagic Stroke – Caused by bleeding from a ruptured vessel in the brain.
- Transient Ischemic Attack (TIA) – A temporary blockage that resolves within 24 hours. Considered a warning sign for future strokes.
How to Recognize a Stroke: The BE FAST Method
Use the BE FAST
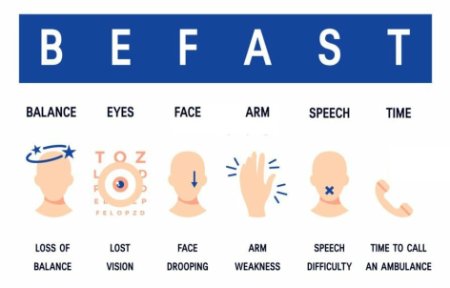
- B – Balance: Sudden loss of balance or coordination. The person may stumble or have trouble walking.
- E – Eyes: Sudden blurred or double vision, or loss of vision in one or both eyes.
- F – Face Drooping: Ask the person to smile. One side of the face may droop or feel numb.
- A – Arm Weakness: Ask them to raise both arms. One arm may drift downward or feel weak or numb.
- S – Speech Difficulty: Ask them to repeat a simple phrase. Speech may be slurred, garbled, or completely absent.
- T – Time to Call 911: If any of these signs are present, even briefly, call 911 immediately. Time lost is brain lost.
Other Warning Signs
- Sudden confusion or difficulty understanding speech
- Sudden trouble seeing in one or both eyes
- Sudden dizziness, loss of balance, or coordination issues
- Severe headache with no known cause
First Aid for Stroke
What to Do While Waiting for Help
- Call 911 immediately—do not delay.
- Keep the person calm and still.
- Have them lie on their side or with head slightly elevated.
- Do not give food, drink, or medication.
- Monitor breathing and be ready to begin CPR if necessary.
When to Call 911
- Any signs of stroke (use the “BE FAST” method).
- Sudden loss of speech, vision, or coordination.
- Seizures, confusion, or loss of consciousness.
- Severe unexplained headache.
Key Takeaways
- Strokes happen when brain cells are deprived of oxygen due to blocked or burst blood vessels.
- Use the “BE FAST” method to identify symptoms quickly and act immediately.
- Calling 911 without delay improves the chance of survival and limits brain damage.
- Do not give anything by mouth. Keep the person still and monitored until EMS arrives.