6.3 BLS for Opioid Overdose
With the rise of opioid-related emergencies, healthcare providers must be prepared to recognize and treat opioid-induced respiratory depression and cardiac arrest. Prompt intervention with rescue breathing, high-quality CPR, and naloxone administration can be life-saving.
Recognizing Opioid Overdose
Opioid overdoses often lead to respiratory arrest before cardiac arrest. Early recognition and intervention can prevent full cardiac arrest.
Key Signs of Opioid Overdose
- Unresponsiveness to voice or pain stimulus
- Slow, irregular, or absent breathing (respiratory depression)
- Pinpoint pupils (miosis)
- Cyanosis (bluish lips, skin, or fingertips)
- Bradycardia (slow heart rate) leading to cardiac arrest if untreated
1. Assess the Patient
- Check for responsiveness by tapping and shouting
- If unresponsive, check for breathing and pulse for no more than 10 seconds
- If the patient has a pulse but is not breathing, begin rescue breathing
- If the patient has no pulse, start CPR immediately
2. Provide Rescue Breathing (If Pulse Is Present)
- 1 breath every 5–6 seconds (~10–12 breaths per minute)
- Use a bag-mask device (BVM) if available
- Each breath should last 1 second and result in visible chest rise
3. Perform High-Quality CPR (If No Pulse)
- Compression rate: 100–120 per minute
- Depth: at least 2 inches (5 cm) in adults
- Minimize interruptions; allow full chest recoil
- Use a 30:2 compression-to-ventilation ratio for single-rescuer CPR
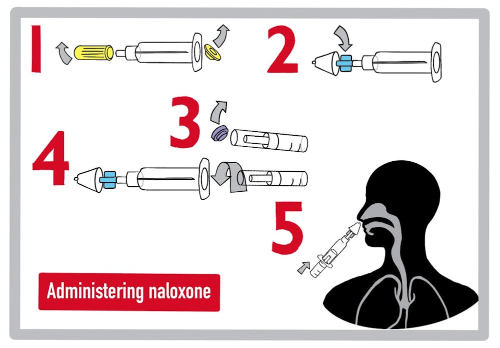
4. Administer Naloxone (Narcan)
Naloxone is an opioid antagonist that can reverse respiratory depression and opioid toxicity.
Naloxone Administration Routes
-
Intranasal (IN):
2–4 mg per spray, repeat every 2–3 minutes as needed×Intranasal (IN):
 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved -
Intramuscular (IM):
0.4–2 mg, repeat every 2–3 minutes as needed×Intramuscular (IM):
 © FAW Training Solutions – All rights reserved
© FAW Training Solutions – All rights reserved - Intravenous (IV): 0.4 mg bolus, titrated to effect
Key Considerations
- If the patient remains unresponsive after 2 doses, continue CPR—opioid overdose may not be the only cause
- Be prepared for withdrawal symptoms if the patient regains consciousness
- Naloxone has a shorter half-life than most opioids—monitor for return of symptoms
Key Takeaways
- Recognize slow breathing, pinpoint pupils, and unresponsiveness
- Provide rescue breathing if the patient has a pulse but is not breathing
- Begin CPR immediately if no pulse is present
- Administer naloxone promptly, and repeat doses as needed
- Monitor closely for recurrent respiratory depression
This concludes the Special Populations section of the HCP BLS course. Up next: a full course recap and certification exam prep.