Real. Fast.
Guaranteed.
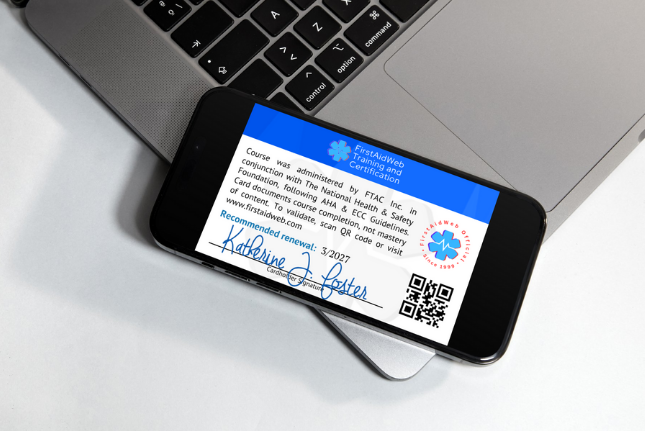
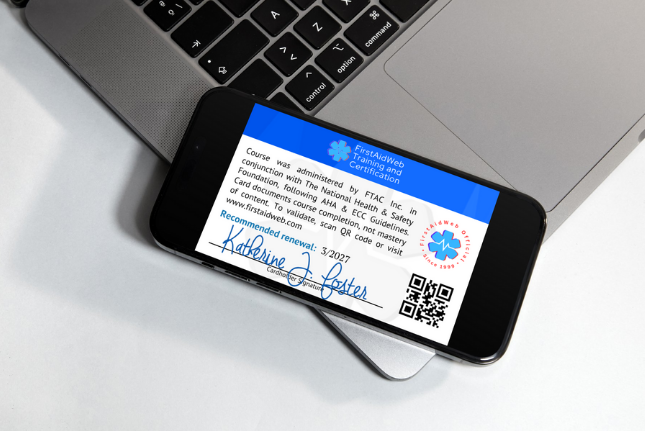
Nationally-accepted 2-year certification card from your own device–in less than an hour!
"...covered everything I will need to work in the school setting and beyond..."

— Chardy Lang
 Verified
★★★★★
Verified
★★★★★
"Awesome course, and easy to understand!!!!! I will recommend this course to my friends in the medical field."

— Rik M.
 Verified
★★★★★
Verified
★★★★★
"Love this so much for my busy lifestyle. Would HIGHLY recommend for anyone."

— Tyson White
 Verified
★★★★★
Verified
★★★★★
Time To Get Certified?
Select Your Course And Start Now
Skip the hassle of classroom training! Whether you need BLS, ACLS, or even PALS, our free online courses let you learn at your own pace—anytime, anywhere. Expertly written, fully compliant, always up to date, and best of all? 100% FREE. Study for free. Take the test for free. And when you pass, pay only if you choose to buy your certification.
CPR & AED for All Age Groups
Ideal for workplace, school, and public responders needing general certification in CPR, AED, and choking response across all age groups
CPR and AED use for victims of all ages, including one- and two-rescuer techniques, choking response, and recovery positioning. Aligned with latest CPR & ECC and ILCOR Guidelines.
 Secure Checkout
Secure Checkout
Universal Emergency First Aid
Designed for both non-medical and professional responders seeking certification in injury, illness, exposure, and other non-CPR emergency response.
Provides foundational instructions for over 25 emergency situations, including protocols for medical, injury-related, and environmental conditions. This comprehensive course is intended for workplace, home, and public use.
 Secure Checkout
Secure Checkout
Healthcare Provider BLS
For clinical and prehospital providers requiring BLS certification in professional care environments
Covers advanced BLS protocols including two-rescuer and team-based CPR, airway management, choking response, opioid overdose, trauma care, and special population considerations. Please note that this course is designed for properly-trained Healthcare Professionals.
 Secure Checkout
Secure Checkout
Adult CPR & AED
For individuals and job roles requiring adult-only CPR and AED certification
Focused on adult-only CPR and AED skills for workplace or organizational compliance. Covers one- and two-rescuer response, choking emergencies, compression protocols, and recovery positioning — aligned with the latest resuscitation guidelines.
 Secure Checkout
Secure Checkout
Trusted Online Certification
All our certification courses meet the cognitive guidelines published by the AHA®/ECC, ILCOR, and OSHA, ensuring compliance with community and workplace requirements.
- 2020-25 AHA CPR & ECC Guidelines
- Accepted In 50 All States
- First Time Certification Or Renewal
- Take Full Course Or Skip To Exam
- Don't Like The Course? Don't Pay!
- No-Questions-Asked Guarantee


Certifying Life-Savers Since 1999
Cloud Based
Nothing To Download Or Install. Secure and Anonymous.
Device Agnostic
For Screens Of All Sizes, At Home Or On-The-Go.
Accepted Worldwide
Adheres To International Industry Standards.

Accepted Or Your Money Back
Official. Instant. Sustainable.
Whether you’re a complete novice or an expert needing to re-certify, we got you covered – study at your own pace, and get certified at your convenience. FirstAidWeb certification is the standard-bearer of online CPR and BLS training and certification.

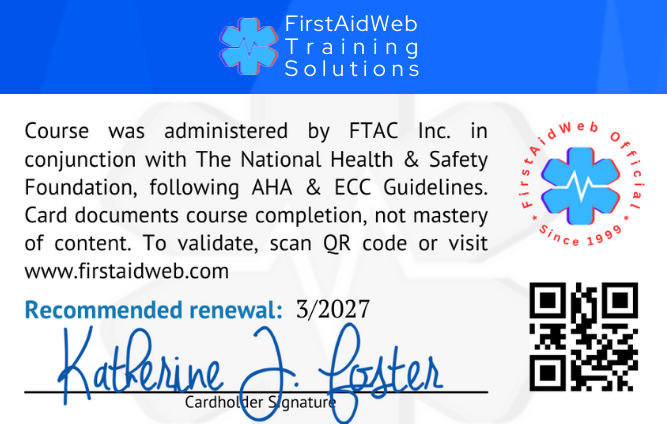
Plastic Is Out. Green Is In.
We all know plastic is bad, and your wallet is already crammed with cards destined for the landfill. So ditch the plastic. Your official digital certification card lives on your device as a versatile PDF—instant, official, and verifiable. Need a hard copy? Print a full-color version anytime from any printer. Same certification you’ve trusted for years with zero environmental cost.
Eco-Friendly
No plastic waste means a cleaner planet for everyone.
Easy Access & Sharing
No waiting for snail mail—download and email your certification instantly.
Always with You
Your wallet card can be saved on your phone so you’re never without it.
ACLS Provider Certification Course
Designed for advanced emergency responders requiring certification in adult cardiac arrest and critical care interventions.
Team-based High-Performance CPR, advanced airway management, ECG rhythm interpretation, defibrillation protocols, and emergency medication administration for adults experiencing cardiac arrest or acute medical emergencies.
 Secure Checkout
Secure Checkout
PALS Provider Certification Course
Designed for healthcare providers treating critically ill or injured infants and children requiring advanced cardiac life support.
Rapid pediatric assessment, high-quality CPR, advanced airway strategies, cardiac rhythm recognition and emergency medication protocols for managing life-threatening situations in infants and children.
 Secure Checkout
Secure Checkout
Why FirstAidWeb?
Our mission is to deliver high-quality, accessible training that empowers individuals with life-saving skills. Our certifications align with established cognitive training guidelines, including those outlined by organizations such as the American Heart Association® (AHA®) / Emergency Cardiovascular Care (ECC), Occupational Safety and Health Administration (OSHA), International Liaison Committee on Resuscitation (ILCOR), and JCAHO.
Eco-Friendly
Easy Access & Sharing
Always with You
Best-Reviewed Provider Since 1999
Pretty straight forward – simple review of information and that was it
Rawly
Best for those coaches and educators prioritizing re-certification.
Eugene Vrana
This course covered everything I will need to work in the school setting and beyond. It was quick and easy without missing out on important topics and information. I will recommend this to others!
Chardy Lang
Easy and very good instructions.
Jay L.
So fast and easy. Thank you.
Susie
Completed the course and took the exam, but got the “Standard First Aid” small card, but the not the “Certificate of Achievement ” . I need this certificate for DCF.
.
June Williams
This certification program is informative and organized.
K.Pierson
Like the self-paced format.
Mike Oesch
Everything great
Isabel Capell
love ittt
Melany Alvarez
Much easier to complete. Thanks
paramjit dhanjal
excellent course
henry sellers
Pretty straight forward – simple review of information and that was it
Rawly
Best for those coaches and educators prioritizing re-certification.
Eugene Vrana
This course covered everything I will need to work in the school setting and beyond. It was quick and easy without missing out on important topics and information. I will recommend this to others!
Chardy Lang
Easy and very good instructions.
Jay L.
So fast and easy. Thank you.
Susie
Completed the course and took the exam, but got the “Standard First Aid” small card, but the not the “Certificate of Achievement ” . I need this certificate for DCF.
.
June Williams
This certification program is informative and organized.
K.Pierson
Like the self-paced format.
Mike Oesch
Ready to Get Certified? Let’s Get This Done!
FirstAidWeb makes getting certified fast, easy, and completely hassle-free. No in-person requirements, no waiting—just complete the course, pass the exam, and download your certificate card instantly.
Instant Certification
100% Online
Guaranteed Accepted
Frequently Asked Questions
Oops!
We couldn't find anything for "".


Didn't Find Your Answer?
We Love Hearing From You!
Have a question or need tech support? Found an error or a broken link? Or maybe you just want to tell us what we’re doing right or where we can improve. Don’t be shy and let us know
